Early Repolarization
Overview
The heart muscle is responsible for circulating blood throughout the body and uses electrical signals from within the heart to manage the heartbeat. When the electrical system of the heart does not operate as it is supposed to, early repolarization (ERP) can develop.
ERP can be seen on an electrocardiogram (EKG). This painless procedure provides a picture of the electrical activity of the heart and how the heart is working. On a normal EKG image, the heart rate will show up as a sudden spike, followed by a smaller, sudden dip and a small gradual incline before leveling off. Patients with ERP will have a different EKG pattern.
ERP was previously thought to be benign; however, recent research suggests that the condition may be associated with the development of life-threatening arrhythmias such as ventricular fibrillation.
Symptoms
Patients with ERP generally do not have any noticeable physical symptoms. The main characteristic associated with the condition is an abnormal pattern on the EKG image. Patients with ERP also often have a lower baseline heart rate.
Causes and Risk Factors
ERP can affect anyone. However, it is most commonly diagnosed in:
- Young adults
- Men
- African Americans
- Athletes
Until recently, because the condition was often associated with healthy young adults and athletes, ERP was considered a benign condition. At times, it was even considered an indication of good health. However, recent studies have linked ERP to the development of life-threatening arrhythmias in some cases.
Diagnosis
ERP is often unintentionally diagnosed when the patient is receiving an EKG for another reason. If an abnormal pattern is seen on the EKG, the physician will generally conduct a physical exam and record the patient's medical history. During the physical exam, the physician will listen to the patient’s heart to detect if there is an abnormal heart rate. Patients are also asked for a detailed description of any symptoms that may be present, as those symptoms may indicate a different heart condition.
In order to rule out other conditions, the physician may order tests to examine the heart muscle, the blood flow through the heart, and any potential leaking within the heart valves. If the abnormal heart rhythm is intermittent, the patient may need to wear a Holter monitor. This portable device allows the medical team to observe the patient’s heart activity over a longer period of time, and it helps diagnose the condition if the abnormal rhythm happens while the patient is not at the hospital.
Depending on the results of the other diagnostic tests, an echocardiogram may be prescribed. This noninvasive procedure uses a machine called a transducer that bounces sound waves off the heart (echo) and back into the transducer. These echoes are then translated into visual images. If the echocardiogram is inconclusive, imaging tests such as a cardiac MRI or chest X-ray may be used to see if the heart is enlarged.
Other diagnostic tests may include electrophysiology studies to look at the electrical system of the heart.
Treatment
If the patient is considered not to be at risk of developing a life-threatening arrhythmia, they may not need treatment. If the patient is considered to be at an increased risk of arrhythmia, then additional treatment methods may be used — including the use of defibrillators, medication or surgery.
Defibrillators implanted in the chest can help manage abnormal electrical impulses that are responsible for ERP. The defibrillator uses two approaches to stop rapid, abnormal heart rhythms. The device can stimulate the heart to beat faster than the abnormal rate — called overdrive pacing — or it can deliver one or more electrical impulses directly to the heart to stop the rhythm.
Medications such as quinidine also work to help the heart be more resistant to abnormal activity. In some cases, a procedure known as catheter ablation uses heat to eliminate the heart's abnormal electrical pathways.
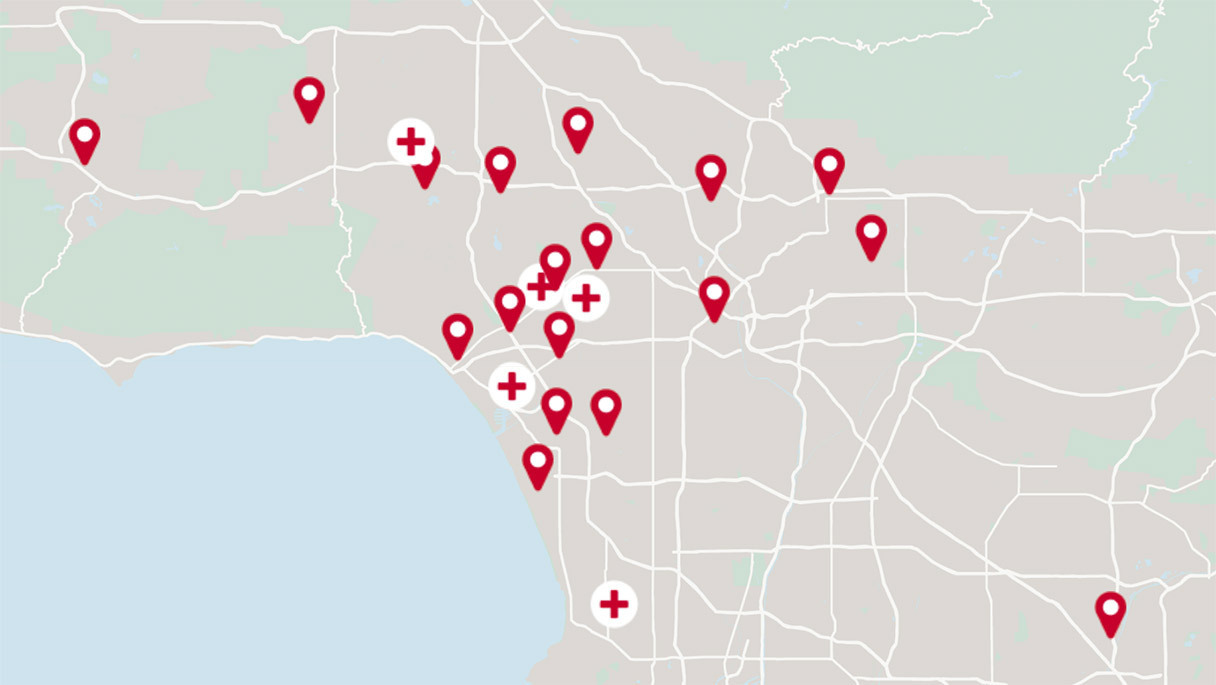
The knowledgeable and highly trained staff at the Cedars-Sinai Heart Institute will work with each patient to determine the best treatment option.
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.