Endometriosis
What is endometriosis?
The tissue that lines the uterus is called the endometrium. Normally, if a woman doesn’t get pregnant, this tissue is shed each month during her period. In endometriosis, tissue that looks and acts like endometrial tissue implants outside the uterus. Each month, this misplaced tissue responds to the hormonal changes of the menstrual cycle. It builds up, breaks down, and bleeds. But, the blood has nowhere to go. This causes surrounding tissue to become inflamed or swollen. It can also cause scar tissue, chronic pain, and heavy periods.
Endometriosis is a main cause of infertility in women. This can happen if the tissue implants in the ovaries or fallopian tubes. Tissue can also implant on other organs in the pelvis and in some cases, outside the pelvis.
What causes endometriosis?
The cause of endometriosis is not clear. It may be that during a woman’s period, some of the tissue backs up through the fallopian tubes into the belly. These cells can implant in the pelvis or be transported through the bloodstream or lymphatics to other parts of the body. Another theory suggests genes are to blame resulting in cells transforming into endometrial tissue. Current research is also looking at the role of the immune system.
Who is at risk for endometriosis?
Any woman may develop endometriosis, but the following women seem to be at an increased risk for the disease:
- Women who have a mother, sister, or daughter with the disease
- Women who gave birth for the first time after age 30
- Women with an abnormal uterus
What are the symptoms of endometriosis?
Each woman may experience symptoms differently, but these are the most common symptoms:
- Pain and cramps that may be felt in the belly or lower back during your period
- Pain during sex
- Abnormal or heavy menstrual flow
- Infertility
- Fatigue
- Painful urination during your periods
- Painful bowel movements during your periods
- Other digestive problems, such as diarrhea, constipation, or nausea
The amount of pain a woman has isn’t always related to the severity of the disease. Some women with severe disease may have no pain. Other women with a milder form of the disease may have severe pain or other symptoms.
How is endometriosis diagnosed?
First, your healthcare provider will review your health history. You will also have a physical exam and a pelvic exam.
A laparoscopy is done to diagnose endometriosis. This uses a thin tube with a lens and a light at the end. It’s inserted into an incision in the abdominal wall to see into the pelvic area. The healthcare provider can often find the locations, extent, and size of the misplaced tissue.
Other tests may include:
- Biopsy. For this test, a small tissue sample is removed from the body and looked at.
- Ultrasound. This imaging test uses high-frequency sound waves to create an image of the organs.
- CT scan. This is an imaging test that uses X-rays and a computer to make detailed images of the body. A CT scan shows details of the bones, muscles, fat, and organs. It can find problems that may not show up on an ordinary X-ray.
- MRI. This imaging test uses a large magnet, radio waves, and a computer to make detailed images of organs or tissue.
How is endometriosis treated?
Your healthcare provider will consider your age, overall health, symptoms and other factors when advising what treatment is best for you. Whether you hope to become pregnant will also play a role in your choices.
Treatment choices include medicine, surgery, or both. If symptoms are mild, you may only need pain medicine. In other cases, hormone-based medicine, such as birth control pills, will stop ovulation and slow endometriosis.
Several choices can be used to remove the implants. Healthcare providers may be able to remove abnormal tissue growths using a laparoscope. In other cases, open surgery is needed. Surgery to remove the uterus (hysterectomy) is also a choice.
What are possible complications of endometriosis?
Endometriosis can make it very hard or impossible for a woman to get pregnant. Sometimes surgery can help. But, in a few cases, women may remain infertile.
Living with endometriosis
Simple steps that can help ease the pain of endometriosis include:
- Rest, relaxation, and meditation
- Warm baths
- Prevent constipation
- Regular exercise
- Use of hot water bottle or heating pad on your belly
Key points about endometriosis
- Endometriosis is common in women during the years they can have children.
- It causes tissue that looks and acts like endometrial tissue to implant outside the uterus.
- Treatment may include medicine, surgery, or both.
- It can make it very hard or impossible for a woman to get pregnant.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
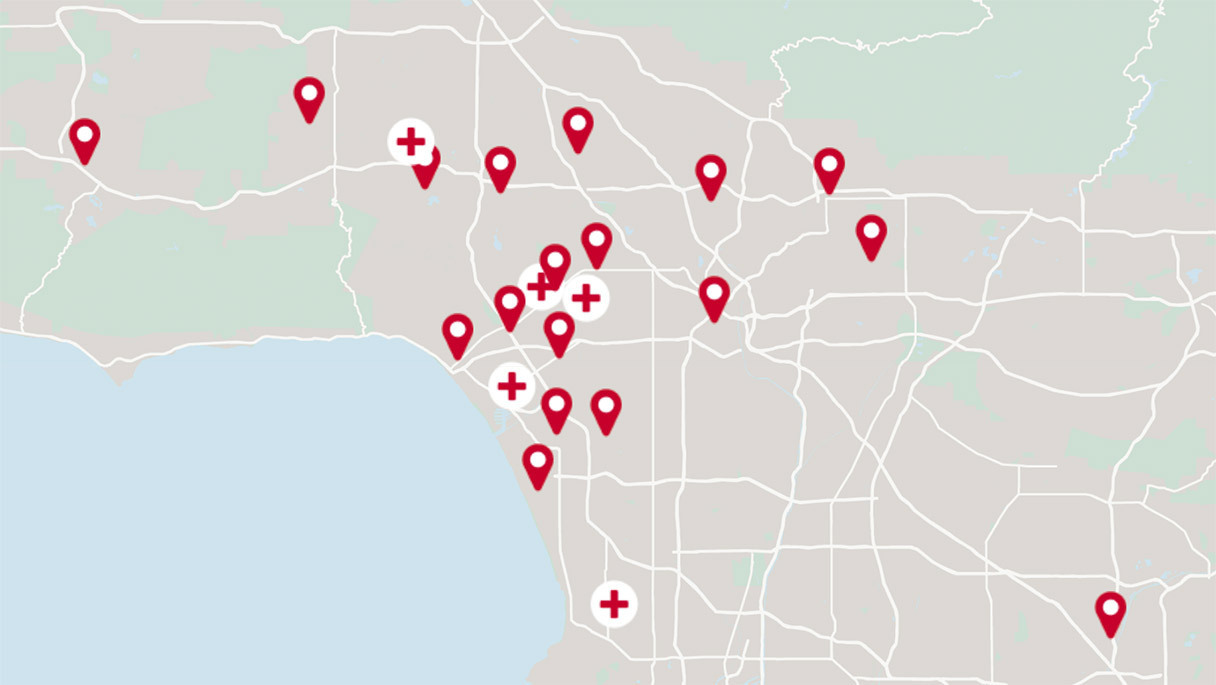
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.