Gestational Diabetes
What is gestational diabetes?
Gestational diabetes is a type of diabetes that happens during pregnancy. Unlike type 1 diabetes, gestational diabetes is not caused by having too little insulin. Instead a hormone made by your placenta keeps your body from using the insulin as it should. This is called insulin resistance. Blood sugar (glucose) then builds up in your blood instead of being absorbed by the cells in your body.
The symptoms of gestational diabetes often go away after delivery. But sometimes they don't. Or you may have a greater risk of developing type 2 diabetes later.
What causes gestational diabetes?
Healthcare providers don't know what causes gestational diabetes. But they do know what happens.
The placenta gives your growing baby nutrients and water. The placenta also makes several hormones to keep the pregnancy healthy. These hormones include:
- Estrogen
- Progesterone
- Cortisol
- Human placental lactogen
These hormones can affect how your body uses insulin (contra-insulin effect). This often begins about 20 to 24 weeks into your pregnancy and could lead to gestational diabetes.
During pregnancy, more fat is stored in your body, you take in more calories, and you may get less exercise. All of these things can make your blood sugar (glucose) levels higher than normal and possibly lead to gestational diabetes.
As the placenta grows, it makes more of the hormones. The risk for insulin resistance becomes greater. Normally your pancreas is able to make more insulin to overcome insulin resistance. But if it can't make enough to overcome the effects of the placenta’s hormones, you can develop gestational diabetes.
Who is at risk for gestational diabetes?
Any woman can develop gestational diabetes during pregnancy. But you may be more likely to get it if you:
- Are overweight or obese
- Have a family history of diabetes
- Are older than 25
- Are African American, American Indian, Asian American, Hispanic or Latino, or Pacific Islander
- Have pre-diabetes (impaired glucose tolerance)
- Have high blood pressure
What are the symptoms of gestational diabetes?
Gestational diabetes doesn't cause any symptoms. That’s why it’s important to get tested for it if you are at high risk.
If your blood sugar levels are very high, you may have these symptoms:
- You urinate more than normal
- You are hungrier or thirstier than normal.
- You have blurred vision
- You have nausea and vomiting
- You lose weight even though you are hungrier
How is gestational diabetes diagnosed?
You should be tested for gestational diabetes in your 24th to 28th week of pregnancy.
The American Diabetes Association also advises that you be tested for type 2 diabetes if you have risk factors for this condition. This testing should be done at your first prenatal visit.
Screening is done by these tests:
- One-hour glucose tolerance test. You drink a special beverage high in sugar. One hour later, the healthcare provider measures your blood sugar (glucose) levels. If your levels are higher than a certain level, this is considered an abnormal result.
- Three-hour glucose tolerance test. If the 1-hour test is abnormal, you will have a second glucose tolerance test done to confirm the diagnosis. You will drink another special beverage, but with more sugar. Your healthcare provider will measure your blood sugar levels 1 hour, 2 hours, and 3 hours later. You have gestational diabetes if at least two of the glucose measurements are higher than normal.
If you are diagnosed with gestational diabetes, you should get tested for diabetes 4 to 12 weeks after your baby is born. You should also get this screening at least every 3 years for the rest of your life.
What is the treatment for gestational diabetes?
You and your healthcare provider will figure out the best treatment for you based on:
- How old you are
- Your overall health and past health
- How sick you are
- How well you can handle specific medicines, procedures, or therapies
- How long the condition is expected to last
- Your opinion or preference
Treatment for gestational diabetes focuses on keeping your blood sugar levels in the normal range. Treatment may include:
- Special diet. You should eat 5 servings of vegetables, fruits, low-fat or nonfat dairy products, and lean meats. Use liquid fats for cooking instead of solid fats. You should eat whole grains and avoid high-calorie snacks or sweet desserts.
- Exercise. You should do moderate exercise unless your healthcare provider tells you not to.
- Daily blood glucose monitoring. Your goal is to keep your blood sugar levels lower than 130mg/dL to 140mg/dL 1 hour after eating.
- Insulin injections. You may need these to control your blood sugar levels. Or you may need other medicines taken by mouth.
What are possible complications of gestational diabetes?
Gestational diabetes usually doesn't cause birth defects. But it can affect your baby in other ways if your blood sugar levels are not under control.
Below are the 2 major health problems that can develop.
Macrosomia
Macrosomia means a baby who is much larger than normal. This happens if the mother’s blood has too much blood sugar in it. The fetus’ pancreas senses this high level of blood sugar and makes more insulin. The fetus then changes the extra blood sugar into fat. This extra fat means a larger baby.
A larger than normal baby can be difficult to deliver. The baby may have trauma or nerve damage, or need to be delivered by cesarean section.
Hypoglycemia
Hypoglycemia is low blood sugar. This can happen to the baby just after he or she is born if the mother’s blood sugar levels are too high. The high levels in the mother cause the fetus to make more insulin. Once the baby is born, he or she no longer has the high blood sugar levels from the mother. This causes the baby’s blood sugar levels to fall very low.
Your blood sugar levels will be watched very closely during labor. Your healthcare provider may give you insulin to keep your blood sugar in a normal range. This will prevent your baby's blood sugar from dropping greatly after delivery.
Babies born to mothers with gestational diabetes may also have low levels of calcium or magnesium in their blood.
These complications can be prevented. The key to prevention is careful control of your blood sugar levels just as soon as the diagnosis of diabetes is made.
Key points about gestational diabetes
- Gestational diabetes is a type of diabetes that happens during pregnancy.
- It may be caused by the hormones made by your placenta. These hormones can make insulin in your body not work as well as it should.
- Gestational diabetes happens about halfway through pregnancy and doesn't cause birth defects.
- If your blood sugar is not under control, your baby can develop problems. One problem is larger growth than normal. The other problem is very low blood sugar just after birth.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
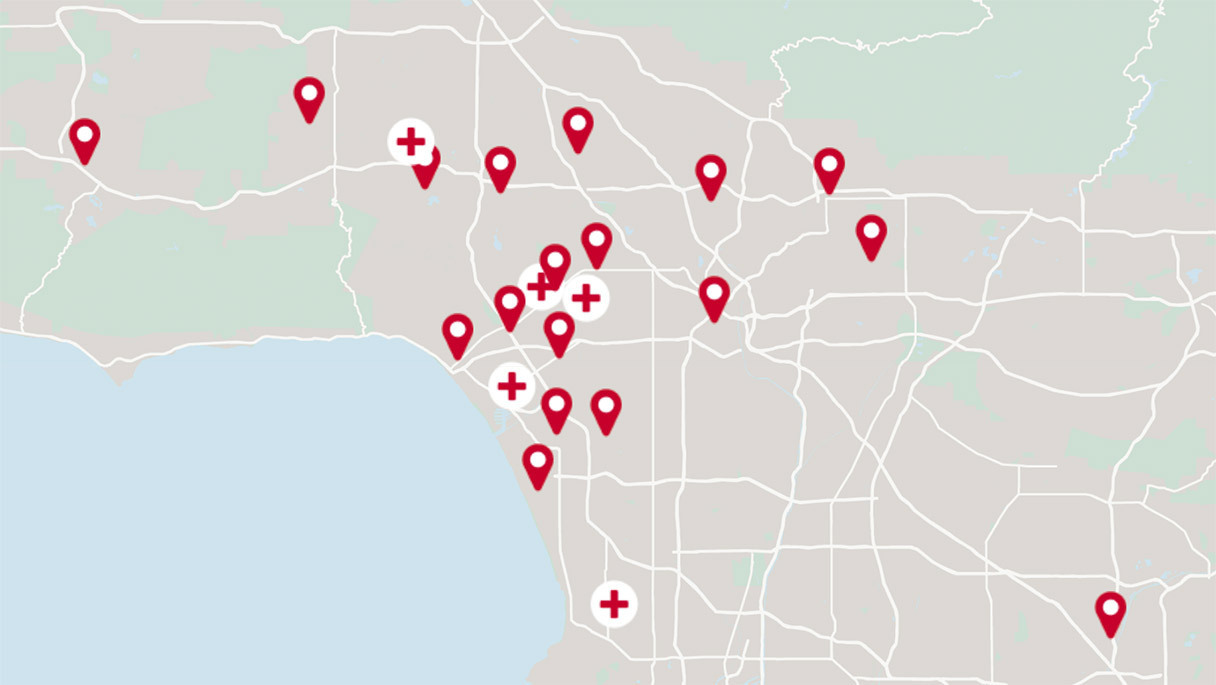
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.