Pleurisy
Overview
Pleurisy, also known as pleuritis, is swelling of the thin lining around the chest cavity and lungs, also known as the pleura. This lining creates a smooth surface so the lungs glide easily in the chest while breathing. When the lining swells, the lungs rub painfully against the chest, causing swelling and chest pain.
In some cases, fluid can collect between the pleura. This is called pleural effusion. When there is no fluid, the condition is called dry pleurisy.
Symptoms
Usually the first sign of pleurisy is a sudden chest pain. The pain may be very mild or very severe. Sometimes the pain is only felt while breathing deeply or coughing. Other times, the pain may be felt all the time and get worse with deep breathing or coughing. Usually the pain is felt in the chest wall over the area that's inflamed. You might also feel pain in the upper abdominal area, neck, back, and shoulders.
Because inhaling deeply hurts, a person with pleurisy tends to breathe quickly and shallowly. On the side where the pain is, the muscles of the chest move less than those on the other side. If fluid builds up between the layers of the pleura, the chest pain may go away. Large quantities of fluid can make expanding one or both lungs difficult.
Other symptoms may include:
- Fever
- Cough
- Shortness of breath
- Rapid breathing
Causes and Risk Factors
Irritation of the pleura can be caused by:
- Viruses
- Bacterial infections
- Cancer
- Inhaling asbestos or other toxic substances
- The use of certain medications
- Some types of autoimmune diseases, such as lupus or rheumatoid arthritis
Diagnosis
Diagnosis of pleurisy usually starts with a physical exam. Because the pain tied to pleurisy is distinct, it is often easy for the physician to diagnose. Using a stethoscope, the doctor may hear a squeaky, rubbing sound.
Chest X-rays and CT scans are often used to see an image of what is going on inside the lungs and chest. These tests help show if fluid is building up in the lungs. They will also show if the lungs are filling up with air as much as possible.
Other imaging tests may be used, such as an ultrasound or electrocardiogram, to rule out heart disease.
If fluid has begun to build up in the chest or lungs, the doctor may take a test sample of it. This will help determine the cause of the pleurisy and rule out the possibility of cancer.
A biopsy of a small sample of tissue may also be done to rule out the possibility of cancer. To do this, a needle will be used to remove a small tissue sample to be examined under a microscope.
A blood test to detect lupus or rheumatoid arthritis may also be performed.
Treatment
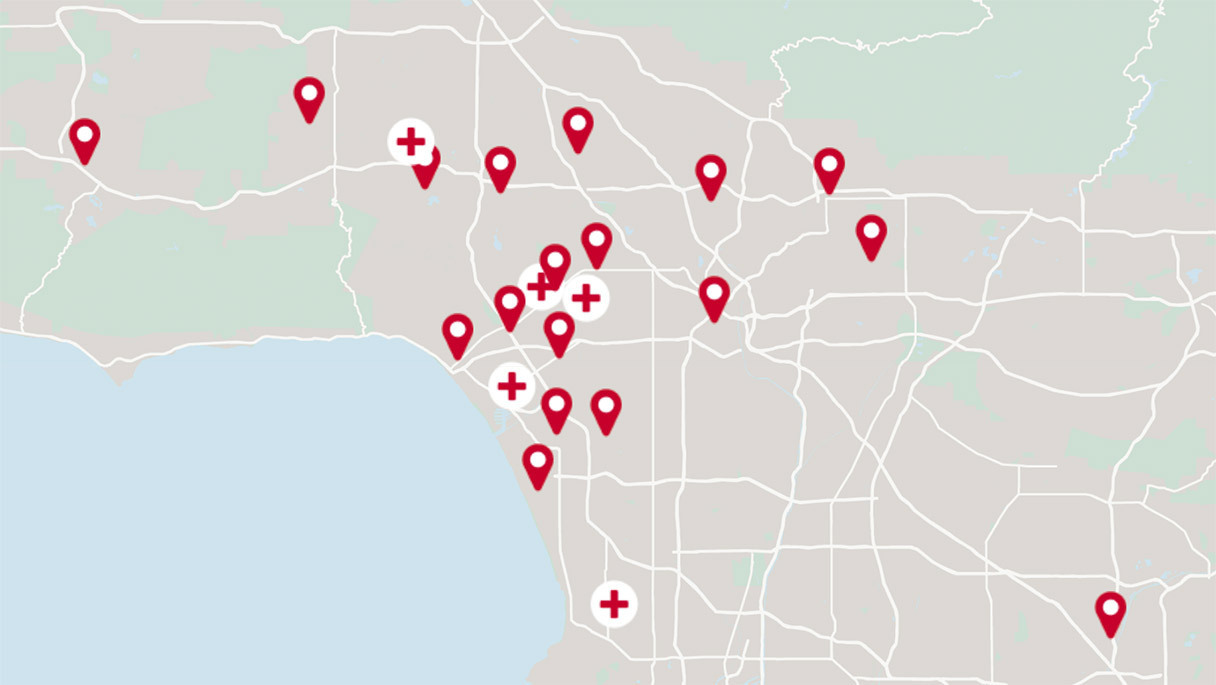
Treatment for pleurisy depends on what caused the condition. The experts at Cedars-Sinai's Advanced Lung Disease Program can help you find the best treatment plan.
Antibiotics may be prescribed for infections caused by bacteria. If a virus causes the pleurisy, no treatment will be given. If the cause is lupus or an autoimmune disease, corticosteroids often quickly cure the pleurisy. These drugs suppress the immune system, which stops the swelling in the lining.
Nonsteroidal anti-inflammatory drugs, such as aspirin or ibuprofen, help relieve the chest pain. Codeine and other stronger pain relievers should not be used. These medicines can stop you from coughing. Coughing is important because it stops the lungs from collapsing and helps prevent pneumonia.
Holding a pillow against the part of the chest that hurts while coughing or breathing deeply can be helpful. Wrapping the chest in wide, elastic bandages can help relieve severe pain. Wrapping the chest also makes it harder to breathe and increases the risk of a collapsed lung or pneumonia.
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.