Pneumonia
What is pneumonia?
Pneumonia is an infection of one or both of the lungs caused by bacteria, viruses, or fungi. It's a serious infection in which the air sacs fill with pus and other liquid.
- Lobar pneumonia affects one or more sections (lobes) of the lungs.
- Bronchial pneumonia affects patches throughout both lungs. It's also called bronchopneumonia.
What causes pneumonia?
There are more than 30 different causes of pneumonia, and they’re grouped by the cause. The main types of pneumonia are:
- Bacterial pneumonia. This type is caused by various bacteria. The most common is Streptococcus pneumoniae. It often occurs when the body is weakened in some way. This may be from illness, poor nutrition, older age, or impaired immunity. Then the bacteria can work their way into the lungs. Bacterial pneumonia can affect all ages. But you are at greater risk if you abuse alcohol, smoke, are weak, have just had surgery, have a respiratory disease or viral infection, or have a weak immune system.
- Viral pneumonia. This type is caused by different viruses, including the flu. It's responsible for about one-third of all pneumonia cases. SARS-CoV-2, the virus responsible for COVID-19 can also cause viral pneumonia. You may be more likely to get bacterial pneumonia if you have viral pneumonia.
- Mycoplasma pneumonia. This type has somewhat different symptoms and physical signs. It's called an atypical pneumonia. It's caused by the bacteria Mycoplasma pneumoniae. It generally causes a mild, widespread pneumonia that affects all age groups.
- Other pneumonias. There are other less common pneumonias that may be caused by other infections including fungi.
Who is at risk for pneumonia?
Anyone can get pneumonia. But the following groups are at the highest risk:
- Adults ages 65 and older
- Children younger than age 2
- People with certain health conditions
- People who smoke or use vaping devices
What are the symptoms of pneumonia?
The symptoms of bacterial pneumonia include:
- Bluish color to lips and fingernails
- Confused mental state or delirium, especially in older people
- Cough that produces green, yellow, or bloody mucus
- Fever
- Heavy sweating
- Loss of appetite
- Low energy and extreme tiredness (fatigue)
- Rapid breathing
- Rapid pulse
- Shaking chills
- Sharp or stabbing chest pain that’s worse with deep breathing or coughing
- Shortness of breath that gets worse with activity
Early symptoms of viral pneumonia are the same as those of bacterial pneumonia, which may be followed by:
- Headache
- Increasing shortness of breath
- Muscle pain
- Weakness
- Worsening of the cough
Mycoplasma pneumonia has somewhat different symptoms. These include a severe cough that may produce mucus.
How is pneumonia diagnosed?
Diagnosis is often made based on your recent health history such as surgery, a cold, or travel exposures. Your healthcare provider will also note the extent of the illness. Based on these factors, your provider may diagnose pneumonia simply on a thorough history and physical exam. These tests may be used to confirm the diagnosis:
- Chest X-ray. This test takes pictures of internal tissues, bones, and organs, including the lungs.
- Blood tests. This test may be used to see if infection is present and if infection has spread to the bloodstream (blood cultures). Arterial blood gas testing checks the amount of oxygen in your bloodstream.
- Sputum culture. This test is done on the material that is coughed up from the lungs and into the mouth. It’s often used to see if there’s an infection in the lungs.
- Pulse oximetry. An oximeter is a small machine that measures the amount of oxygen in the blood. A small sensor is taped or clipped onto a finger. When the machine is on, a small red light can be seen in the sensor. The test is painless and the red light does not get hot.
- Chest CT scan. This imaging procedure uses a combination of X-rays and computer technology to make sharp, detailed horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than regular X-rays.
- Bronchoscopy. This is direct exam of the main airways of the lungs (bronchi) using a flexible tube (bronchoscope). It helps to check and diagnose lung problems, assess blockages, and take out samples of tissue or fluid for testing,
- Pleural fluid culture. In this test, a fluid sample is taken from the pleural space. This is the space between the lungs and chest wall. A long, thin needle is put through the skin between the ribs and into the pleural space. Fluid is pulled into a syringe attached to the needle. It's sent to the lab where it’s tested to find out which bacteria is causing the pneumonia.
How is pneumonia treated?
Treatment depends on the type of pneumonia you have. Most of the time, pneumonia is treated at home. But severe cases may be treated in the hospital. Antibiotics are used for bacterial pneumonia. Antibiotics may also speed recovery from mycoplasma pneumonia and some special cases. Most viral pneumonias don’t have specific treatment. They often get better on their own.
Other treatment may include eating well, increasing fluid intake, getting rest, oxygen therapy, pain medicine, fever control, and maybe cough-relief medicine if cough is severe. If you smoke or use vaping devices, talk to your doctor about ways how to stop.
Can pneumonia be prevented?
Check with your healthcare provider about getting vaccines. The flu is a common cause of pneumonia. So getting a flu shot every year can help prevent both the flu and pneumonia.
There are also 2 pneumococcal vaccines. They will protect you from a common form of bacterial pneumonia. Children younger than age 5 and adults ages 65 and older should get a shot.
The pneumococcal shot is also recommended for all children and adults who are at greater risk for pneumococcal disease because of other health conditions.
The risk of COVID-19 transmission can be reduced through: washing your hands frequently, avoiding large crowds, staying 6 feet away from people who don’t live in your immediate household, and wearing a mask.
What are possible complications of pneumonia?
Most people with pneumonia respond well to treatment. But pneumonia can be very serious and even deadly.
You are more likely to have complications if you are an older adult, a very young child, have a weak immune system, or have a serious health problem such as diabetes or cirrhosis. Complications may include:
- Acute respiratory distress syndrome (ARDS). This is a severe form of respiratory failure.
- Lung abscesses. These are pockets of pus that form inside or around the lung. They may need to be drained with surgery.
- Respiratory failure. This requires the use of a breathing machine or ventilator.
- Sepsis. This is when the infection gets into the blood. It may lead to organ failure.
Key points about pneumonia
- Pneumonia is an infection of one or both of the lungs caused by bacteria, viruses, or fungi.
- Anyone can get it. But those at highest risk include children younger than age 2, adults 65 and older, people who smoke, and people with certain health conditions.
- The most common symptom is a cough that produces green, yellow, or bloody mucus. Other symptoms include fever, shaking chills, shortness of breath, low energy, and extreme tiredness.
- Pneumonia can often be diagnosed with a health history and physical exam. Tests used to look at the lungs, blood tests, and tests done on the sputum you cough up may also be used.
- Most people with pneumonia respond well to treatment, but pneumonia can cause serious lung and infection problems. It can even be deadly.
-
The risk of getting COVID-19 viral pneumonia can be reduced through: washing your hands frequently, avoiding large crowds, staying 6 feet away from people who don’t live in your immediate household, and wearing a mask.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your healthcare provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your healthcare provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare if you have questions.
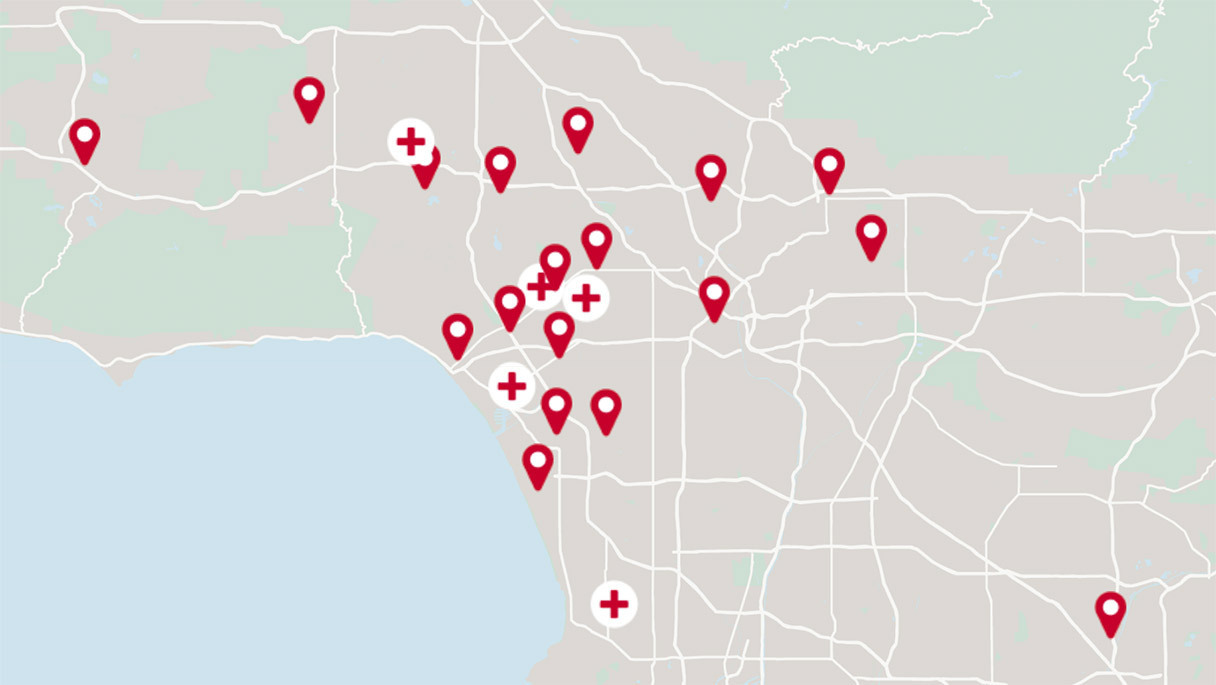
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.