Psoriatic Arthritis
What is psoriatic arthritis?
Psoriatic arthritis is a type of arthritis linked with psoriasis, a chronic skin and nail disease. Psoriasis causes red, scaly rashes and thick, pitted fingernails. Psoriatic arthritis is similar to rheumatoid arthritis (RA) in symptoms and joint swelling (inflammation). But it tends to affect fewer joints than RA. And it does not make the typical RA antibodies. The arthritis of psoriatic arthritis comes in 5 forms:
- Arthritis that affects the small joints in the fingers, toes, or both
- Asymmetrical arthritis of the joints in the hands and feet
- Symmetrical polyarthritis, which is similar to RA
- Arthritis mutilans, a rare type of arthritis that destroys and deforms joints
- Psoriatic spondylitis, arthritis of the lower back (sacroiliac sac) and the spine
What causes psoriatic arthritis?
Doctors don't know what causes psoriatic arthritis. But factors such as immunity, genes, and the environment may play a role.
What are the symptoms of psoriatic arthritis?
The psoriasis symptoms may start before or after the arthritis. Psoriasis causes red, scaly rashes and thick, pitted fingernails. Up to 3 in 10 people with psoriasis may develop psoriatic arthritis. Symptoms of psoriatic arthritis may include:
- Inflamed, swollen, and painful joints, often in the fingers and toes
- Deformed joints from chronic inflammation
The symptoms of psoriatic arthritis can look like other health conditions. Make sure to see your healthcare provider for a diagnosis.
How is psoriatic arthritis diagnosed?
Psoriatic arthritis is easier to confirm if you already have psoriasis. If you don’t have the skin symptoms, diagnosis is more difficult. The process starts with a health history and a physical exam. Your healthcare provider will ask about your symptoms. You may have blood tests to check the following:
- Erythrocyte sedimentation rate (ESR or sed rate). This test looks at how quickly red blood cells fall to the bottom of a test tube. When swelling and inflammation are present, the blood’s proteins clump together and become heavier than normal. They fall and settle faster at the bottom of the test tube. The faster the blood cells fall, the more severe the inflammation.
- Uric acid. High blood uric acid levels can be seen in psoriatic arthritis but are not used for diagnosis or monitoring.
- Imaging tests. X-rays, CT scans, ultrasound, MRI, and skin biopsies may all be used to help diagnose psoriatic arthritis.
How is psoriatic arthritis treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on the severity of your condition.
Both the skin condition and the joint inflammation are treated. Early diagnosis and treatment help prevent joint damage. Some medicines used to treat psoriatic arthritis include:
- Nonsteroidal anti-inflammatory medicines (NSAIDs) to ease symptoms
- Corticosteroids for inflammation
- Immunosuppressive medicines such as methotrexate to reduce inflammation if NSAIDs don't work
- Biologic medicines to ease inflammation
- Vitamins and minerals such as calcium and vitamin D to slow bone deformation
Other treatment may include:
- Exercise
- Heat and cold
- Occupational therapy to help you do your daily activities
- Physical therapy to help your muscle and joint function
- Management of psoriasis skin rash
- Splints
- Surgery to repair or replace a damaged joint. This is usually not needed until years after diagnosis.
- Ultraviolet light treatment (UVB or PUVA)
What are possible complications of psoriatic arthritis?
The condition may damage joints enough to change your activity level. Lack of activity can lead to stiff joints and muscle weakness. Psoriatic arthritis can also cause tiredness (fatigue) and low red blood cell count (anemia). You are more likely to develop:
- Diabetes
- High blood pressure
- High cholesterol
- Obesity
Living with psoriatic arthritis
There is no known cure for psoriatic arthritis. But you can help manage your symptoms by sticking to your treatment plan. Manage pain with medicine, acupuncture, and meditation. Get enough exercise. Good exercises include yoga, swimming, walking, and bicycling. Work with a physical or occupational therapist. They can suggest devices to help you in your daily tasks.
When should I call my healthcare provider?
Let your healthcare provider know if your symptoms get worse or you have new symptoms.
Key points about psoriatic arthritis
- Psoriatic arthritis is a form of arthritis with a skin rash.
- Psoriasis is a chronic skin and nail disease. It causes red, scaly rashes and thick, pitted fingernails. The rash may come before or after the arthritis symptoms.
- Psoriatic arthritis causes inflamed, swollen, and painful joints. It happens most often in the fingers and toes. It can lead to deformed joints.
- Treatment may include medicines, heat and cold, splints, exercise, physical therapy, and surgery.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions.
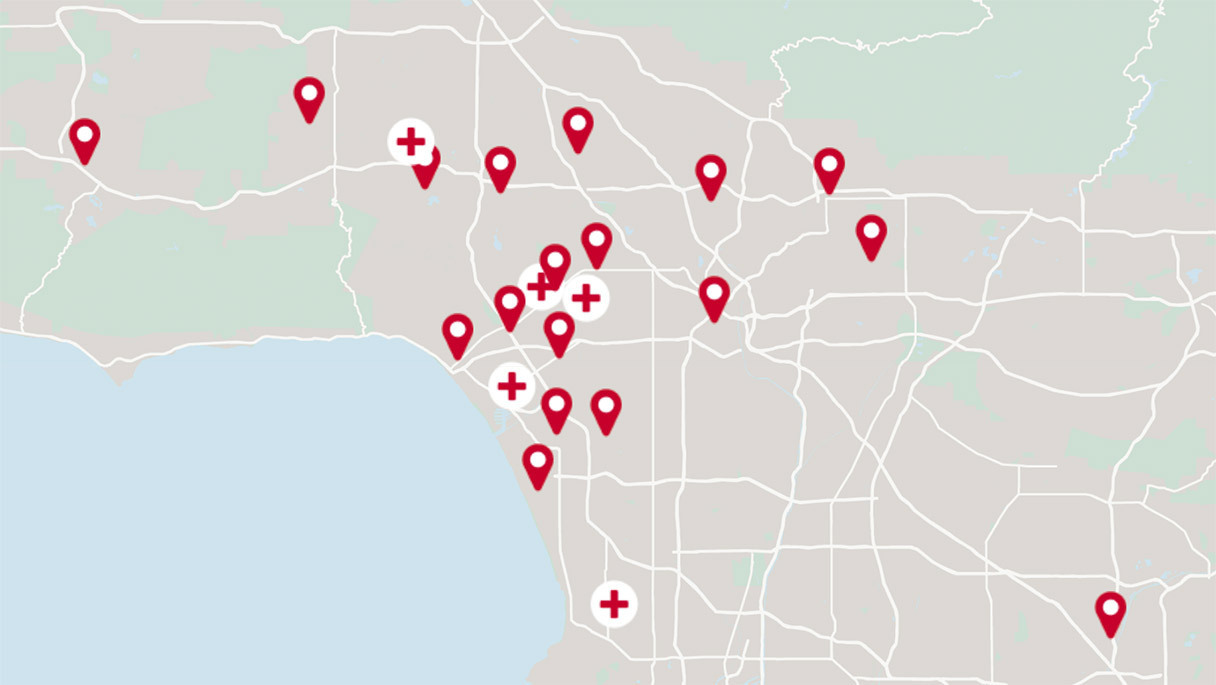
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.