Rheumatic Fever
What is rheumatic fever?
Rheumatic fever is a complication of a strep throat. Fighting off the strep infection can cause other parts of the body to develop swelling or inflammation. This can happen even to those parts of the body that aren't directly infected by the virus.
One common and potentially dangerous effect of rheumatic fever is damage to the valves of the heart. This can lead to narrowed or leaky heart valves. The mitral (or bicuspid) valve, which permits blood to flow from the left atrium to the left ventricle of the heart, is affected most often. The aortic valve is frequently affected. The tricuspid and pulmonic valves are rarely affected.
What causes rheumatic fever?
It is not yet known what causes rheumatic fever. It appears that when some people's bodies fight off a strep throat infection, other parts of the body develop inflammation (swelling and tenderness).
Research has focused on whether this is an abnormal response by the immune system to the antigens produced by some types of streptococcal bacteria. The possibility that some people have a genetic disposition to have this response is also being studied.
What are the risk factors for rheumatic fever?
Your risk of developing rheumatic fever is greater if you:
- Are between the ages of 6 and 15 years
- Are a woman. The disease is twice as common in women as it is in men.
- Are in a situation where you have a greater chance of being exposed to streptococcus infections, such as in a developing country where there is not enough food, overcrowding and poverty.
- Have had previous rheumatic fever or evidence of rheumatic heart disease.
While it is relatively rare in the United States, there have been outbreaks over the last 20 years that tended to occur in white, middle-class suburban neighborhoods or in rural areas. Additionally, more aggressive strains of streptococci appear to be returning to the United States.
What are the symptoms of rheumatic fever?
Rheumatic fever develops only after a person has had a strep infection, which causes symptoms such as:
- Fever
- Headache
- Muscle aches
- Red and swollen tonsils
- Sore throat
If you have a sore throat and fever for more than 24 hours or have a severe sore throat without much fever or other cold symptoms — especially if you've been exposed to someone with a strep infection — you should see your doctor. Rheumatic fever is easier to prevent than treat.
Prompt treatment of a strep infection can prevent the development of rheumatic fever. In more than half of all cases, rheumatic fever may affect the heart valves (rheumatic carditis) and interfere with blood flow through the heart.
Even without treatment, though, only about three people out of every 10 who have a strep throat infection develop rheumatic fever. The signs of rheumatic fever usually appear about five weeks after the strep infection.
Symptoms of rheumatic fever are divided into major and minor. A doctor will make a diagnosis of rheumatic fever if:
- Two major signs are present, or
- One major and two minor signs are present in person who has had a strep infection
The major symptoms are:
- Inflammation (swelling) of your heart. About half the time people have a first attack of rheumatic fever, they develop this. If this happens, you may feel weak or short of breath, or have chest pain. A physical examination or a test such as an electrocardiogram or chest X-ray may also indicate inflammation of the heart. The inflammation may not lead to permanent damage, but it can lead to scarring of the heart valves and damage severe enough to cause heart failure. Sometimes the damage isn't diagnosed until years after the rheumatic fever has gone away.
- Pain that moves from joint to joint. This can cause painful swelling, redness and a feeling of heat.
- A lack of coordination or uncontrollable jerky movements of your arms, legs and face. Your handwriting may become worse, for example. This symptom is known as chorea, Sydenham's chorea, rheumatic chorea or St. Vitus' dance. About one out of every 10 people who have rheumatic fever develops this. It usually disappears in a few weeks or months.
- Pink or faint red rashy patches that don't itch on your skin.
- Lumps under the skin, even if the rash isn't there.
The minor symptoms include:
- A blood test indicating inflammation
- Abnormal heartbeat on an electrocardiogram
- Fever
- Heart murmurs that hadn't been present before
- Joint pain without inflammation
How is rheumatic fever diagnosed?
No single test can confirm a diagnosis of rheumatic fever.
It is important that your doctor make sure that your symptoms aren't caused by gout, sickle cell anemia, leukemia, embolic bacterial endocarditis, drug reactions or arthritis, all of which can have symptoms similar to those of rheumatic fever.
Your doctor will usually do a physical examination and take your medical history. During the exam, the doctor will look for achy, painful joints, swelling, rashes or lumps on your skin and shortness of breath. They will check your heart for murmurs that weren't there before.
If the heart is involved, it is important that your doctor distinguish whether the symptoms you are experiencing are caused by rheumatic carditis instead of birth defects of the heart that also cause heart murmurs. Additionally, juvenile rheumatoid arthritis can sometimes begin suddenly and affect the heart in ways similar to that of rheumatic fever.
An electrocardiogram (EKG) may show abnormal heart rhythms.
Because a diagnosis of rheumatic fever requires evidence that you have had a recent strep infection, your doctor may order a blood test to check for antibodies to streptococcal bacteria.
How is rheumatic fever treated?
Treatment will vary depending on the symptoms, how severe they are and whether there is damage to the heart. Generally, treatment consists of getting rid of any remaining strep bacteria and treating the symptoms.
Treatment may include:
- Limiting your activity to manage joint pain, chorea or symptoms of heart failure.
- Pain relievers such as codeine or nonsteroidal anti-inflammatory drugs (NSAIDS) such as aspirin to relieve mild joint pain. More aggressive pain relievers may be needed if the pain is severe.
- NSAIDs such as aspirin to control inflammation if you have carditis.
- Corticosteroids such as prednisone for severe carditis, especially if it is associated with symptoms of heart failure.
- Antibiotics such as penicillin to assure that no streptococcal bacteria are left behind. It may be necessary to take antibiotics for years to prevent another attack of rheumatic fever. Without this precaution, additional attacks of rheumatic fever are common for three to five years after the first infection.
People who develop valve disease will need to take antibiotics before having dental work, oral surgery or surgery involving the chest and lungs, the intestines or the genital or urinary tracts.
Key points
- Rheumatic fever is a complication of a strep throat. About three people out of every 10 who have a strep throat infection develop rheumatic fever.
- One common and potentially dangerous effect of rheumatic fever is damage to the valves of the heart.
- No single test can confirm a diagnosis of rheumatic fever.
- Generally, treatment consists of getting rid of any remaining strep bacteria and treating the symptoms.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
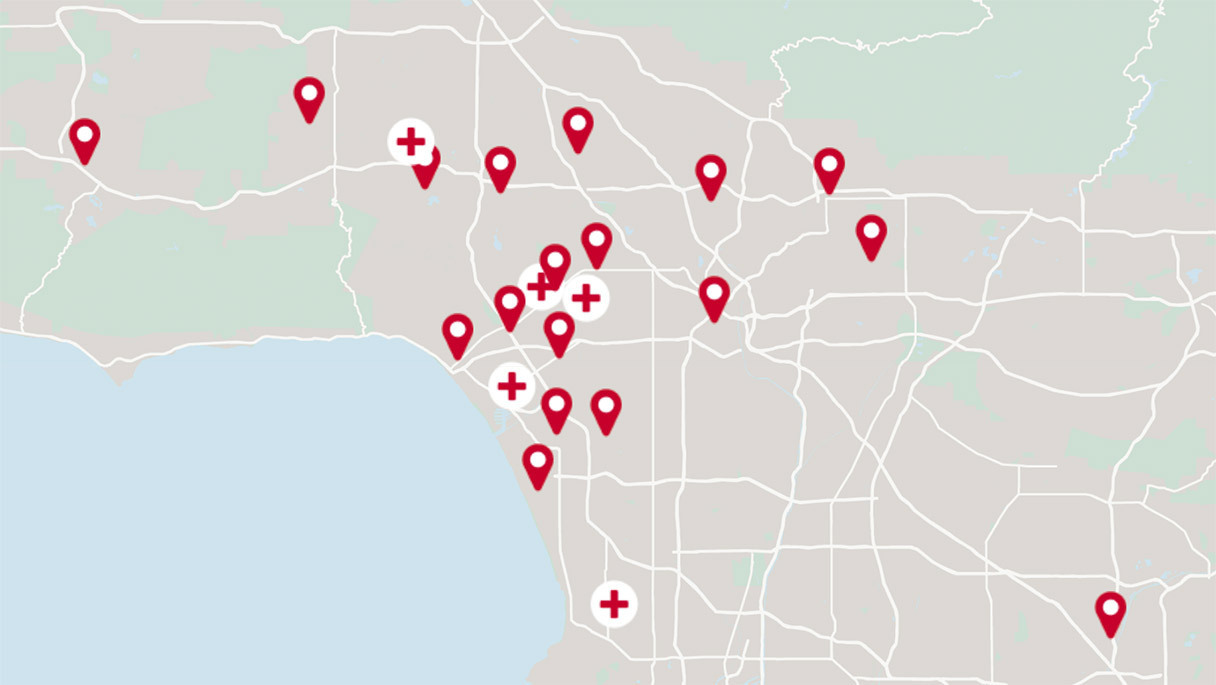
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.