Scleroderma
What is scleroderma?
Scleroderma is a rare, long-term (chronic) disease that causes abnormal growth of connective tissue. It can affect the joints, skin, cartilage, and internal organs. It is degenerative and gets worse over time. The disease can be in one part of the body. This is called localized scleroderma. Or it may affect the whole body. This is a more serious condition called systemic sclerosis. Scleroderma is more common in women.
What causes scleroderma?
Scleroderma is thought to be an autoimmune disease. This means the symptoms are caused by the body attacking its own healthy tissues. Genes play a role in the disease, but the environment may also play a role. Family members of people with scleroderma have a mildly increased risk of developing scleroderma. But many people with scleroderma don't have family members with the condition.
What are the symptoms of scleroderma?
Scleroderma can lead to scarring of the skin, joints, and internal organs. Symptoms can be a bit different for each person, and may include:
- Calcium bumps on the fingers or other bony areas
- Grating noise as inflamed tissues move
- Heart failure and abnormal heart rhythms
- Immovable fingers, wrists, or elbows because of scarring, hardening, and tightening of the skin
- Joint pain
- Kidney disease
- Pale and tingly fingers that may turn numb when exposed to cold or during emotional upset (Raynaud’s phenomenon)
- Scarring of the esophagus. This leads to heartburn and trouble swallowing.
- Scarring of the lungs. This leads to shortness of breath.
- Sores on fingertips and knuckles
- Spider veins
- Tight, shiny, darker skin on large areas that may cause problems with movement
- Fingertips get thick and swollen
The symptoms of scleroderma can look like other health conditions. Always see your healthcare provider for a diagnosis.
How is scleroderma diagnosed?
The process starts with a health history and a physical exam. Diagnosis is based on the changes in the skin and internal organs. An antibody test may help show the type of scleroderma. You may need tests such as:
- Electrocardiogram (ECG). This test records the electrical activity of the heart, shows abnormal rhythms, and detects heart muscle damage. An ECG may be done to find changes in the heart muscle tissue caused by scleroderma.
- Echocardiogram. This test uses sound waves to create a moving image of the heart and its valves. It is done to look at the structure and function of the heart.
- X-ray. This test uses a small amount of radiation to create images of internal tissues, bones, and organs. X-rays may show changes in bone, soft tissues, and organs caused by scleroderma.
- CT scan. A CT scan uses X-rays and a computer to produce detailed images of the body. It may be done to check for interstitial lung disease or bone abnormalities.
How is scleroderma treated?
Treatment will depend on your symptoms, age, and general health. Treatment may include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) or corticosteroids to ease pain
- Penicillamine to slow the skin thickening process and delay damage to internal organs
- Immunosuppressive medicines, such as methotrexate
- Treatment of certain symptoms, such as heartburn and Raynaud’s phenomenon
- Physical therapy and exercise to maintain muscle strength
Talk with your healthcare providers about the risks, benefits, and possible side effects of all medicines.
What are possible complications of scleroderma?
With localized scleroderma, some symptoms may get better over time. But damage to skin and other organs may be lifelong (permanent). With systemic sclerosis, symptoms can over time lead to damage to the skin and cause thickened, tight skin. This may change the way you look and cause problems with your movement. It can also cause severe kidney, lung, digestive, or heart problems. In severe cases, these organ problems can lead to death.
Living with scleroderma
Systemic scleroderma is a long-term (chronic) condition. It is important that you learn ways to best manage your symptoms. Learn about the disease and work with healthcare providers who have experience with scleroderma. Scleroderma can affect many systems of the body. So you may need to have many specialists on your healthcare team. Physical and occupational therapists may help you with managing your activities of daily living. Make sure that you and other team members are in regular touch with each other. If you can't manage your care, pick a trusted person to oversee your care. Make sure to address your emotional well-being, too. Don't hesitate to ask for help when you need it.
When should I call my healthcare provider?
If your symptoms get worse or you have new symptoms, let your healthcare provider know.
Key points about scleroderma
- Scleroderma is a rare, long-term condition that causes abnormal growth of connective tissue. It can affect the joints, skin, cartilage, and internal organs.
- Symptoms can include joint pain, skin hardening and thickening, scarring of the lungs and esophagus, pale and tingly fingers, and kidney disease.
- It can affect one area of the body. In more severe cases it affects the whole body.
- It occurs more often in women.
- There is no known cure. Treatment is focused on easing pain and slowing down further damage to the body.
Next steps
Tips to help you get the most from a visit to your healthcare provider:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your healthcare provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions.
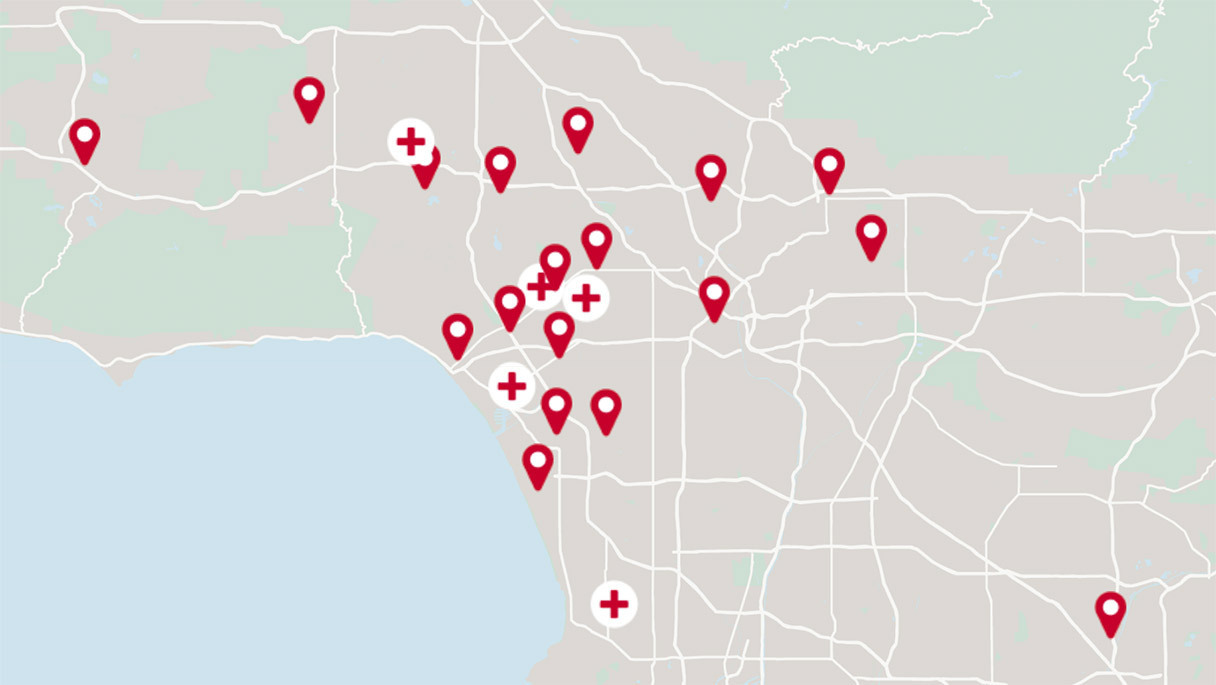
Get the care you need from world-class medical providers working with advanced technology.
Cedars-Sinai has a range of comprehensive treatment options.