July 2024 Case
Case Presentation
A patient in their late 60’s presented to our institution with a history of refractory DLBCL diagnosed elsewhere. At the time of his initial diagnosis, CT scan of the patient's chest, abdomen, and pelvis showed diffuse lymphadenopathy and hepato-splenomegally. Axillary lymph node biopsy showed an atypical lymphoid infiltrate diagnosed as Diffuse Large B-cell Lymphoma (DLBCL), germinal center type. Bone marrow biopsy showed involvement by lymphoma. Patient was treated with R-CHOP and radiation therapy, which was complicated by chemotherapy induced heart failure.
Six months later, the patient presented to an outside institution complaining of fatigue and weight loss. Imaging, lab workup, and bone marrow biopsy showed relapse/ progression of the patient's disease. Patient was treated with steroids, discharged in stable condition, and referred out for expert consultation and assessment of candidacy for CAR-T cell therapy. Patient was admitted to our institution for R-ICE chemotherapy induction as a bridge to CAR-T cell therapy and discharged pending further evaluation. However, patient presented two days later with hypothermia and pancytopenia.
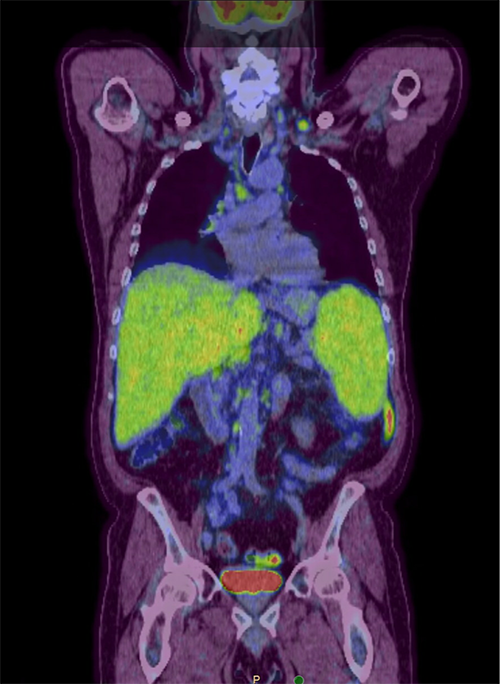
A PET-CT showed Multiple areas of increased activity in supraclavicular lymph nodes bilaterally.
HISTOLOGY, IMMUNOHISTOCHEMISTRY, FLOW CYTOMETRY IMMUNOPHENOTYPING, MOLECULAR, AND CYTOGENETIC STUDIES:
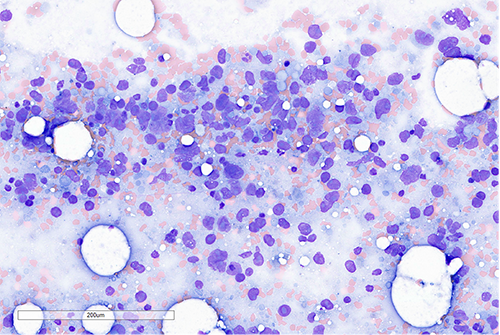
Bone marrow aspirate smear was hypocellular and paucispiculate. In areas with preserved cellularity, large atypical cells with giant pleomorphic nuclei and prominent macronucleoli are identified.
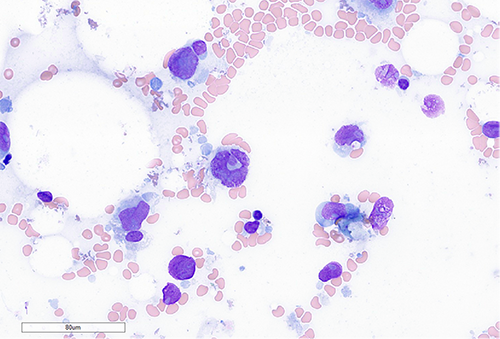
A higher power view of the atypical cells.
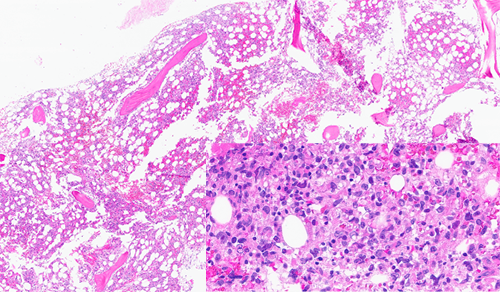
Bone marrow core biopsy showed a packed fibrotic marrow with large atypical lymphoid cells with large pleomorphic nuclei and abundant cytoplasm (shown inset on high-power). Some areas showed a spindled morphology.
However, immunohistochemistry and immunophenotyping by flow cytometry were not consistent with a B-cell lymphoma. The large atypical cells were positive for histiocytic markers such as CD68, CD163, CD4, lysozyme, S100, and IRF8. Cytogenetic studies, including Fluorescent in-situ hybridization (FISH) showed amplification of BCL2 and BCL6 and Next-generation sequencing (NGS) showed mutations of NOTCH2 and SOCS1 with deletions in CDKN2a, ETV6, and CIC. B-cell receptor heavy and light chain gene rearrangement studies by PCR were positive as were studies for T-cell receptor gene rearrangement.
Diagnosis
The case was sent from our institution for outside consultation, which agreed with our diagnosis of histiocytic sarcoma, transformed from DLBCL.
Discussion
Although the lesional cells lost immunophenotypic expression B-cell markers and instead expressed those of a histiocytic sarcoma, they retained their original genetic signature, which was picked up by our cytogenetic and molecular testing methods. As mentioned earlier, FISH showed amplification of MYC and BCL6, which are specifically associated with aberrant somatic hypermutation of germinal center B cells in the setting of lymphoma. And NGS showed mutations in NOTCH2, which is essential for terminal B cell differentiation and mediates cellular crosstalk in lymphomas, as well as SOCS1, which is a negative regulator of the JAK/STAT3 pathway and has a strong association with DLBCL.
This rarely-reported phenomenon of transformation of a lymphoid neoplasm, to that of a lymphoid-associated mesenchymal lineage such as follicular dendritic cell, or histiocyte gives further credence to the hematopoietic cell of origin theory and the concept of a common myeloid-lymphoid progenitor. A similar phenomenon of a clonal relationship between angio-immunoblastic T-cell lymphoma and subsequently developed myeloid neoplasms has been reported.
Treatment of these neoplasms has been complicated by frequent development of tumor resistance with most patients showing a poor response to chemotherapy. A combination of newer generation BRAF and MEK inhibitors has shown favorable outcome in small studies, and some studies showing response to EGFR inhibitors, and PD-1 blockade. Median survival is currently 6 months- 1 year despite treatment. Our patient did not tolerate the chemotherapy bridge to CAR-T and died of heart failure a few weeks after induction.
References
- Evans MG and Kim AS. The Hematologist 2021:18(1)
- Lewis NE, et al. Blood Adv 2020;4:2261
- Tiacci E et al. NEJM 2018;379;981
- Cheng S, et al eLife 2021;10:e66395
- Cox N, et al. Annu. Rev. Immunol 2021;39;313
- Journal of the National Comprehensive Cancer Network 20, 6; 10.6004/jnccn.2022.7001