October 2024 Case
Clinical History
Patient in G2P1 at 32 weeks 0 days gestational age with breech presentation presented to labor and delivery of Cedars Sinai Medical Center with decreased fetal movement for one day. Pregnancy course was otherwise uncomplicated. Bedside ultrasound revealed absence of fetal heart tones consistent with intrauterine fetal demise (IUFD). After discussion with the patient, cesarean was performed. An autopsy was requested.
Autopsy Findings
The gross examination of the fetus revealed fusion and lymphedema of the second, third, and fourth fingers of the right hand, with loss of the distal parts of these fingers; fusion of the second and third toes of the left foot; constrictions of the distal parts of the second and third toes of the left foot and the middle part of the fourth toe of the right foot, with amniotic bands around the constrictions; and constriction grooves on both lower extremities.

Figure 1. Constrictions and fusions of digits, toes, and lower extremities
Microscopic examination of fetal organs identified vascular congestion and interstitial hemorrhage of lung parenchyma, moderate degree of stress induced thymic involution and nucleated red blood cells in fetal circulation, indicative of intrauterine fetal hypoxia.
Histological examination of the placenta revealed characteristic features of high-grade fetal vascular malperfusion (including vascular ectasia, extensive thrombosis of chorionic plate and stem villous vessels, stem villous vessel obliteration, focal villous stromal vascular karyorrhexis, and villous dysmaturity) as well as signs of amniotic band syndrome (ABS), such as the absence of the amnion in the fetal membranes and chorionic plate.
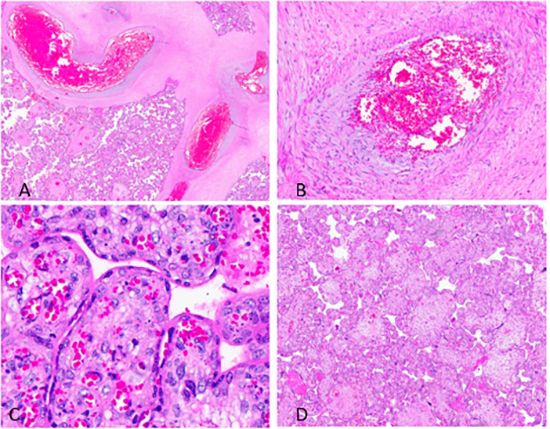
Figure 2. Features of fetal vascular malperfusion in placenta. (A) Vascular ectasia. (B) Vascular thrombus. (C) Villous stromal vascular karyorrhexis. (D) Villous dysmaturity
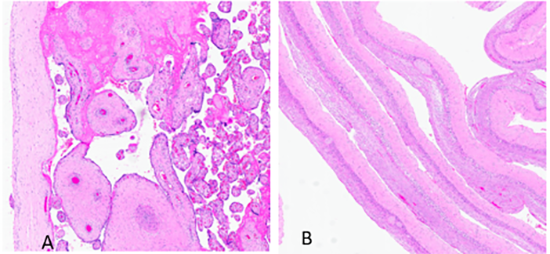
Figure3. Features of amniotic band syndrome in placenta. (A) Absence of the amnion in the fetal membranes. (B) Absence of the amnion in the chorionic plate
Diagnosis
Fetal vascular malperfusion in the setting of amniotic band syndrome.
Discussion
Amniotic band syndrome (ABS) is characterized by a group of congenital anomalies that occur in association with bands of amniotic epithelial lined connective tissue extending from the fetal surface of the placenta, potentially encircling fetal parts and umbilical cord. Three patterns of abnormalities can be seen in this syndrome: placenta denuded of amnion with thickened chorion; fetal attachments or entanglements by fibrous bands or amniotic remnants; and fetal malformations, deformations, and/or disruptions which do not conform to any identifiable syndrome. All these features were identified in the current case.
The incidence of ABS has been reported to range between 1 in 1200 to 1 in 15000 live births in various studies. The exact etiology is unknown, but the most widely accepted hypothesis is tearing of amnion with temporary loss of amniotic fluid and fusion of chorion and mesodermal amnion resulting in entrapment of fetal parts. This is a sporadic disorder, with no known genetic implications and most cases occurring in chromosomally normal fetuses.
The most typical fetal anomalies associated with ABS are constricted or amputated extremities and digits. Strips of amnion or chorion connective tissue become attached to the limbs or digits, often encircling them and leading to constriction or amputation. When pregnancy terminates in the second trimester, intact bands of amnion can be seen running between chorionic sac and the affected area. However, in more mature fetuses like this case continuity is lost and few degenerate threads remain, although a complete encircling band may be identified applied to a limb constriction defect. Other congenital anomalies associated with ABS include abnormalities of craniofacial region including anencephaly, exencephaly and complex facial clefts; thoraco-abdominal wall defects including omphaloceles; and limb malformations including pseudosyndactyly, clubbed feet and abnormal dermatoglyphics.
Amniotic bands may also encircle and constrict the umbilical cord. An amniotic band was observed attached to umbilical cord in this case and could have played a role in fetal vascular malperfusion (FVM) and potential restriction of umbilical blood flow. However, no anatomic constriction was identified. Therefore, it is not possible to determine if amniotic band syndrome was the cause of FVM in this case. Nonetheless, there was clear FVM and the pattern and distribution were indicative of umbilical cord flow obstruction problem. On histologic examination of thymus, moderate degree of stress induced thymic involution was identified, which is an indication of intrauterine fetal distress.
Also, the presence of nucleated red blood cells in the fetal circulation is an abnormal finding and is characteristically seen in association with intrauterine fetal hypoxia, which in this case most likely was a result of FVM.
FVM is a common cause of IUFD, particularly in the third trimester of pregnancy, and is the most likely mechanism of fetal demise in this case. In many instances the causative mechanism or specific umbilical cord abnormality is not identified. Of note, amniotic band syndrome as well as FVM are most often incidental with no significant increased risk of recurrence in subsequent pregnancies.
References
- Redline RW, Boyd TK, Roberts DJ. Placental and Gestational Pathology. Cambridge University Press; 2018.
- Roberts DJ, Polizzano C, American Registry of Pathology. Atlas of Placental Pathology. American Registry of Pathology; 2021.
- Wigglesworth JS, Singer DB. Textbook of Fetal and Perinatal Pathology.
- Khong TY, Malcomson RDG, eds. Keeling’s Fetal and Neonatal Pathology. Fifth edition. Springer; 2015. doi:10.1007/978-3-319-19207-9
- Cignini P, Giorlandino C, Padula F, Dugo N, Cafà EV, Spata A. Epidemiology and risk factors of amniotic band syndrome, or ADAM sequence. J Prenat Med. 2012 Oct;6(4):59-63. PMID: 23272276; PMCID: PMC3530965.
- Rushton DI. Amniotic band syndrome. Br Med J (Clin Res Ed). 1983 Mar 19;286(6369):919-20. doi: 10.1136/bmj.286.6369.919. PMID: 6403134; PMCID: PMC1547338.
- Boyd TK. Increased Circulating Fetal Nucleated Red Blood Cells. In: Redline RW, Boyd TK, Roberts DJ, eds. Placental and Gestational Pathology. Diagnostic Pediatric Pathology. Cambridge University
